Last Updated: September 8, 2025
In vitro fertilization (IVF) is an assisted reproduction technique where eggs are collected, fertilised with sperm in a laboratory, and 1–2 resulting embryos are transferred to the uterus. It can help when other treatments fail, especially with blocked fallopian tubes, male‑factor infertility, endometriosis, PCOS, premature ovarian failure (with donor eggs), or unexplained infertility. Success depends on age, diagnosis, and method.
What is IVF – Summary
- What IVF is: Lab fertilisation of eggs with sperm, embryo culture for 2–5 days, then embryo transfer. Extra embryos are commonly frozen for future use.
- Who it helps: Blocked/absent fallopian tubes, low ovarian reserve/ageing (often with egg donation), male‑factor infertility (often with ICSI), endometriosis, PCOS, premature ovarian failure (donor eggs), unexplained infertility.
- Success: Declines after 35 with own eggs; donor‑egg outcomes are age‑independent (per cited report ranges below).
- Law & access: Policies vary by country on age limits, marital status, donor anonymity, embryo transfer limits, testing, freezing, and surrogacy.
What is IVF treatment?
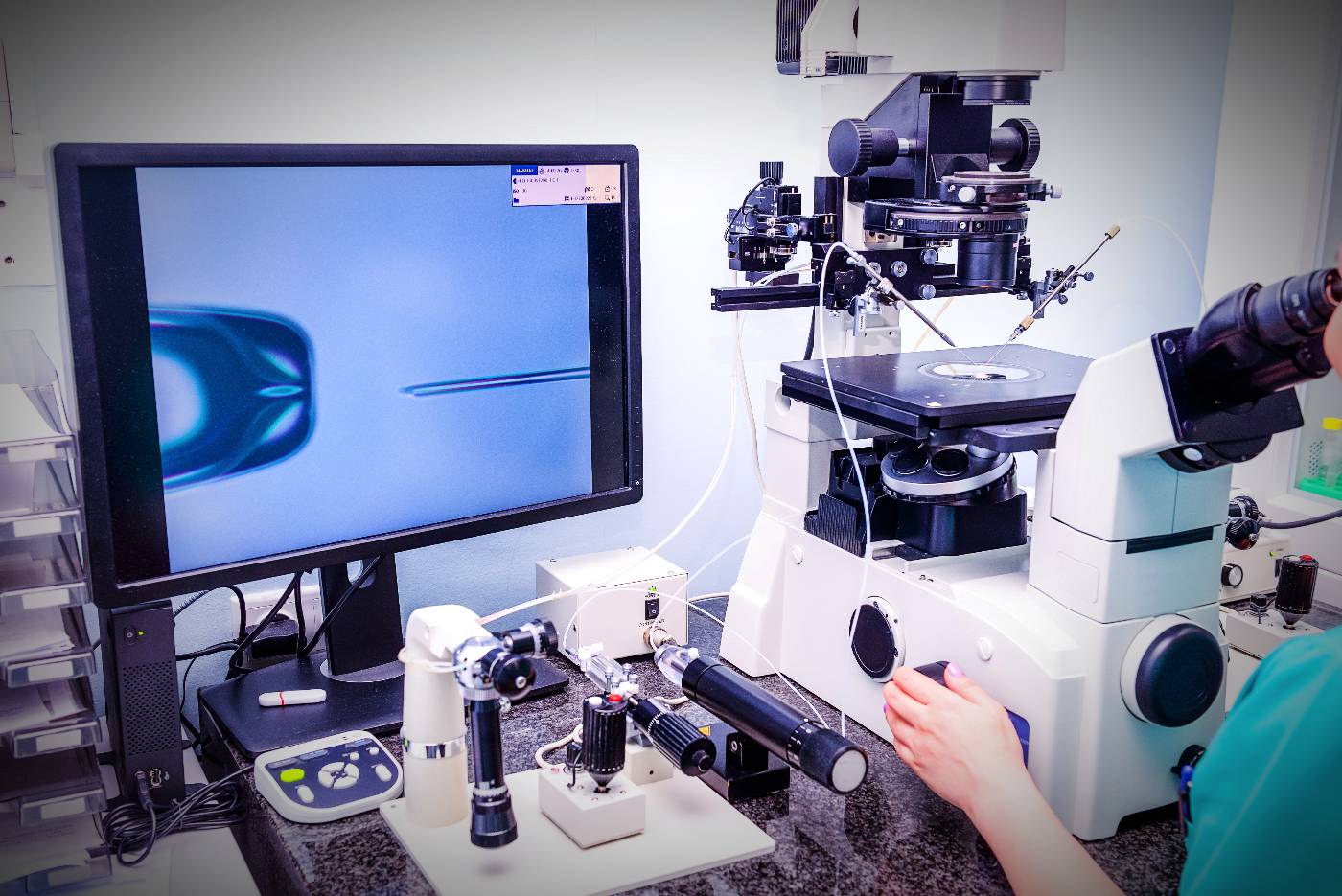
IVF is an assisted reproduction technique involving oocyte fertilisation by a sperm sample in the in vitro laboratory.
Core steps:
- Ovarian stimulation (hormone therapy) to develop several follicles.
- Egg collection and fertilisation in a lab (“test tube”).
- Embryo culture in an incubator for 2–5 days.
- Embryo transfer (usually 1–2 embryos) through the vagina into the uterus.
- Implantation and potential pregnancy.
Freezing: Because not every transferred embryo implants, additional embryos are frozen (now standard in most IVF clinics) for later attempts if needed.
When can IVF help?
IVF is not usually the first step in infertility care. It’s typically considered after fertility drugs, artificial insemination, and/or surgery have not led to pregnancy.
Common scenarios where IVF can help:
- Blocked or absent fallopian tubes: IVF bypasses the tubes, enabling pregnancy with your own eggs.
- Ageing or low ovarian reserve: IVF can raise the chance of conceiving; when eggs are too few or low quality, egg donation can be used.
- Male‑factor infertility: IVF with ICSI (intracytoplasmic sperm injection) addresses low count, motility, morphology, physical blockage, prior vasectomy, or past IVF failures.
- Endometriosis: IVF has shown success, including some severe cases.
- PCOS: For hormone imbalance leading to irregular cycles, IVF can help when medication response is poor.
- Premature ovarian failure/menopause: Donor eggs can provide high success potential.
- Unexplained infertility: IVF often succeeds when a clear diagnosis is lacking.
Quick guide: You generally need only one healthy sperm to fertilize an egg with IVF‑ICSI.
Can IVF always help?
Not in every situation. For example, if a woman cannot produce healthy eggs and opts not to use donated eggs, success chances are low.
Age matters:
- After 37, chances with your own eggs decline.
- Approaching the 40s, using donor eggs may boost chances. Donor‑egg IVF tends to give similar chances across age groups, though miscarriage risk increases after 40.
Medical factors that can reduce effectiveness:
- Ovarian/uterine dysfunctions and abnormalities
- Fibroid tumors
- Hormone level abnormalities
- Genetic abnormalities (oocytes, sperm, embryos)
Advantages of IVF with ICSI
Why consider ICSI? Male‑factor infertility is common, and ICSI is a powerful add‑on to IVF. Even with female‑factor issues, pregnancy rates with IVF+ICSI can be as high or higher than with standard IVF.
Situations where ICSI can help:
- Low sperm count
- Past IVFs without success
- Physical blockage
- Poor sperm morphology or motility
- Prior vasectomy
Bottom line: ICSI gives couples a route to fertilisation even in severe male‑factor cases.
General IVF treatment options
Different paths suit different clinical situations. Here’s a concise tour of options mentioned.
IVF with own eggs
Eggs are collected and fertilised with partner’s or donor’s sperm; pre‑embryo is transferred to the uterus. Suits healthy‑egg scenarios with male‑factor issues or damaged/blocked tubes, and for couples after failed artificial insemination.
Natural IVF cycle
No stimulating fertility drugs; the single egg from your normal cycle is collected and fertilised.
Pros: No hyperstimulation drugs (no OHSS risk from stimulation), fewer medication side effects, may align with personal/religious beliefs about storing/destroying surplus eggs/embryos, and no long wait between cycles if a try fails.
Cons: Lower success rates than standard stimulated IVF.
Mild stimulation IVF
Uses fewer fertility drugs and for a shorter duration.
Definition reference: “Mild ovarian stimulation is the administration of fixed, low doses of gonadotrophins in GnRH antagonist cycles and/or the use of anti‑estrogens or aromatase inhibitors with the aim of limiting the outcome to no more than eight oocytes retrieved.” (Best practices of ASRM and ESHRE, Human Reproduction, 2012)
Key points:
- Smaller and shorter drug exposure; fewer menopausal‑like side effects.
- Often yields fewer eggs collected.
- Shorter time between attempts.
- Success data vary because protocols differ by patient.
- Combining mild stimulation with elective single embryo transfer (eSET) may preserve delivery rates per cycle while reducing downsides of aggressive stimulation.
IVF with donor eggs (oocyte donation)
For women who cannot get pregnant with own eggs due to absence or low quality. Donor eggs are fertilised in the lab and embryos are transferred to the uterus. The recipient is not genetically related, but is the birth mother on record.
Sperm donation
A donor provides sperm for insemination via clinic/sperm bank or privately. Most women choose artificial insemination with donor sperm; some choose natural insemination believing it raises chances. Common among heterosexual couples with male‑factor infertility or single women.
IVF for single mother
A single mother may be widowed, unmarried, or divorced. Some single women choose single motherhood using donor sperm.
IVF for same‑sex parents
Same‑sex couples can become parents through adoption, surrogacy, or (for female couples) pregnancy using donated sperm. The topic remains controversial in many countries, and same‑sex marriage is still banned in some.
Surrogacy
An arrangement where a woman carries a pregnancy for a couple or single intended parent—used when carrying a pregnancy is medically unsafe or impossible.
- Embryo source: Intended parents’ eggs/sperm, donor eggs/sperm, or a mix.
- Partial surrogacy: Embryo created with intended father’s sperm and surrogate’s eggs.
When IVF fails: what next?
It’s common to need more than one cycle. Data cited indicate around 3 IVF cycles per live birth on average for patients below 40.
First, take a breath: Don’t rush immediately into another attempt. IVF is demanding physically and emotionally. Recovery time—with support from loved ones—can help and may improve future chances.
Why reflection matters: IVF can act as a prognostic exercise, revealing how you respond to stimulation and embryo development. Identifying factors linked with failure at each stage helps refine decisions about continuing.
Five must‑dos after a failed cycle:
- Review outcomes with the clinic team—what likely went wrong?
- Ask your clinician and embryologist about chances in a next cycle.
- Discuss different approaches that could improve odds.
- Talk through innovations in IVF—even if not available locally, your doctor should inform you of options.
- See a counsellor to process feelings and clarify next steps.
Evidence referenced notes that multiple failed IVF‑ET cycles are not necessarily linked to a lower chance of success next time.
Legal aspects of IVF you should know
The legal landscape can feel like a maze. Policies differ by country and region, and personal or religious beliefs add complexity.
How is IVF regulated?
- Fertility care is governed by ethical and legal policies—with particularly high stakes because it helps create new life.
- Some countries have laws; others rely on regulatory guidelines; some have no explicit rules, leaving decisions to clinics.
Issues commonly regulated:
- Eligibility: Age limits differ. One country may deny IVF due to age, while another permits it.
- Marital status: Some countries (e.g., China, Turkey, Indonesia) require marriage. Others (e.g., USA, Sweden, Spain) allow IVF for single women and same‑sex couples. Female same‑sex couples are often legally recognised as parents; male couples may be parents only in limited circumstances via surrogacy.
- Number of oocytes to fertilise: Some places cap the maximum.
- Donor anonymity: In the UK, donors are not fully anonymous; many patients travel to Spain, where donors are anonymous.
- Embryo development time: Some countries permit only early embryo transfer; others allow several days of development.
- PGT‑A/PGS & PGD: Many allow PGD for genetic disease screening; some ban it.
- Embryos transferred: Single embryo transfer is increasingly common; some countries still allow multiple embryo transfer.
- Embryo freezing period: Permissible storage time is often regulated.
- Surrogacy: Rules and processes vary widely.
What is IVF?
An assisted reproduction technique where eggs are fertilised with sperm in a lab, embryos are cultured for 2–5 days, and 1–2 are transferred to the uterus; extra embryos are typically frozen.
When should I consider IVF?
After fertility drugs, artificial insemination, or surgery have not worked—especially with blocked tubes, male‑factor infertility, endometriosis, PCOS, premature ovarian failure (donor eggs), or unexplained infertility.
How many embryos are transferred?
Often one (single embryo transfer is recommended by regulators) or two; remaining embryos can be frozen for later.
Does age affect success?
Yes. Success with own eggs declines after 35 and more after 37–40. Donor eggs can make outcomes age‑independent, though miscarriage risks rise with age.
What are the main risks?
Medication effects (including OHSS), multiple pregnancy (mitigated by SET), miscarriage, rare ectopic pregnancy, rare retrieval complications, and a slightly higher birth‑defect rate vs natural conception.
What is ICSI and who needs it?
Intracytoplasmic sperm injection places a single sperm into an egg—useful for severe male‑factor cases and after prior IVF failures.
What happens if IVF fails?
Take time to recover, review with your team, discuss alternative approaches and innovations, and consider counselling. Multiple failed cycles do not necessarily predict failure next time.
Are there legal limits?
Yes—on age, marital status, donor anonymity, embryo numbers, testing, freezing, and surrogacy. Policies vary by country.
Further reading: