Polycystic Ovary Syndrome or PCOS is a hormonal imbalance that affects 5 to 10 percent of women of reproductive age across the world, and results in irregular or absent periods, acne, excess body hair and weight gain. Polycystic Ovary Syndrome is also a major cause of infertility and yet is frequently misdiagnosed and often missed completely.
Polycystic Ovary Syndrome gets its name because, under an ultrasound scan, the ovaries can look like a bunch of grapes, each one covered in what look like multiple cysts. In fact, these aren’t cysts at all but are small, undeveloped follicles.
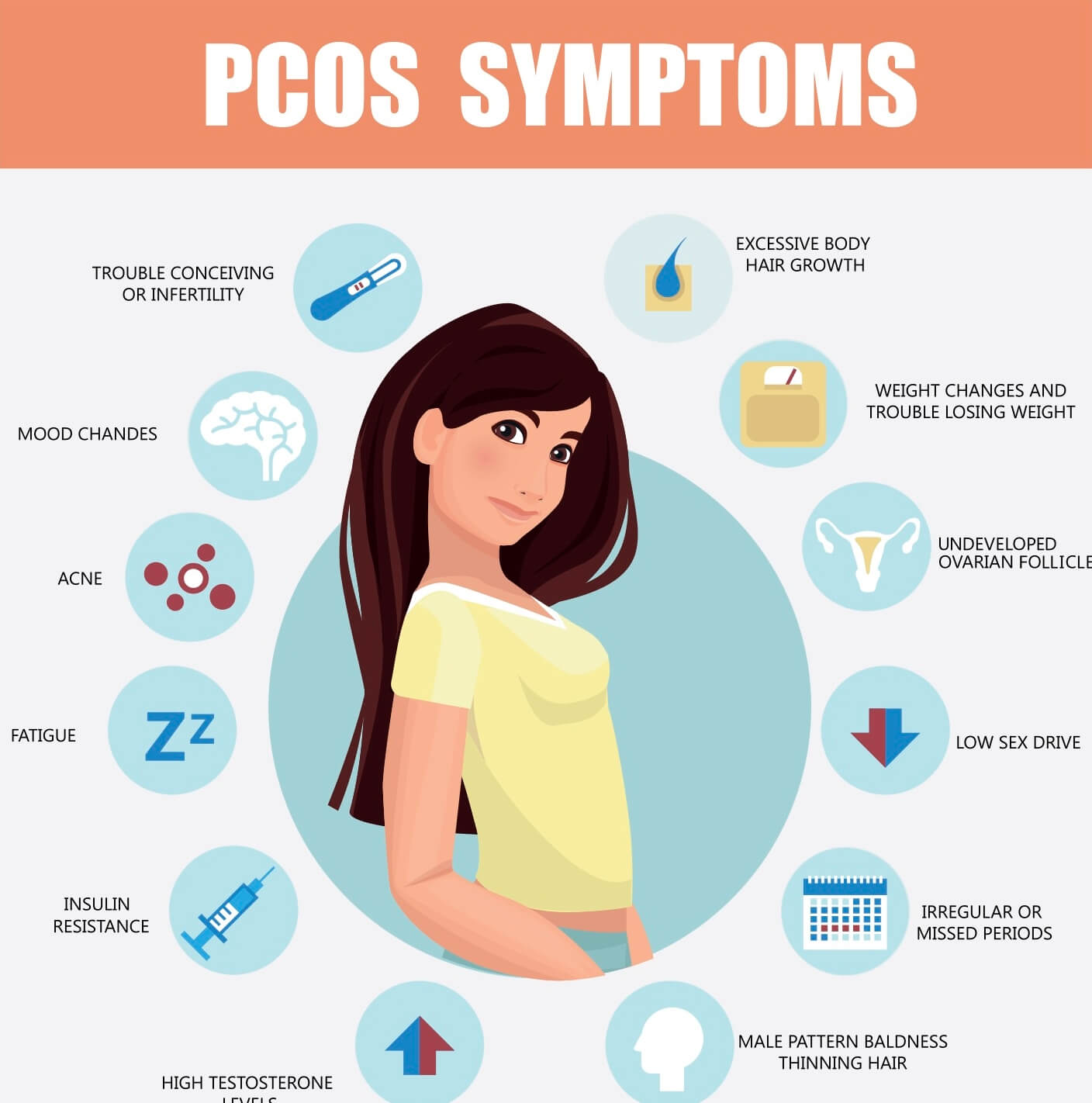
Not every woman with PCOS will get the same symptoms, but there are common symptoms you should look out for.
Common symptoms of PCOS include:
- Few or no periods
- Excess hair on the face or breasts or inside of the legs or around the nipples
- Acne
- Oily skin
- Scalp hair thinning or loss (male pattern baldness)
- Skin tags (known as acrochordons)
- Skin discolouration (known as acanthosis nigricans) where the skin looks ‘dirty’ on the arms, around the neck and under the breasts
- Mood swings
- Depression
- Lack of sex drive
- Weight gain especially around the middle of the body
- Difficulty in losing weight
- Cravings and binges
- No or irregular ovulation
- Difficulty in becoming pregnant
- Recurrent miscarriages
PCOS creates a vicious cycle of hormone imbalances, which has huge knock-on effects throughout the rest of your body. With PCOS, the problem often starts with the ovaries, which are unable to produce the hormones they should, and in the correct proportions. But linked to this is the very common problem of insulin resistance.
Women with PCOS very often have difficulties with blood sugar levels which can cause weight gain and the excess insulin can stimulate your ovaries to produce yet more testosterone.
Half of all women with PCOS do not have any problems with their weight, yet they can still have higher insulin levels than normal.
How is Polycystic Ovary Syndrome diagnosed?
The most widely accepted criteria for the diagnosis of PCOS says that you should have two out of these three problems:
- Infrequent or no ovulation
- Signs (either physical appearance – hirsutism or acne – or blood tests) of high levels of male hormones
- Polycystic ovaries as seen on an ultrasound scan
The Seven Nutritional Steps to beat Polycystic Ovary Syndrome
Good nutrition is the foundation of your health and you should never underestimate how powerful it can be. It is the fuel that provides you with the energy to live your life and it gives your body the nutrients it needs to produce your hormones in the correct balance. The better the supply of those nutrients, the more healthily your body will function.
The fundamental aim of my nutritional approach to PCOS is to target a number of areas simultaneously so that you get the maximum effect in the minimum amount of time.
Here’s how:
- Switch to unrefined carbohydrates (eaten with protein) and never go more than 3 hours without food to keep your blood sugar levels balanced
- Eat oily fish and foods rich in Omega 3s to help your body to become more sensitive to insulin so it can overcome insulin resistance
- Cut out all dairy products for 3 months to bring levels of male hormones under control
- Eat more vegetables and pulses to which helps control male hormones
- Cut right back on or cut out alcohol for 12 weeks to allow your liver function to improve
- Cut down on caffeine to give your adrenal glands a rest
- Cut down on saturated fats and eliminate trans fats to help control the potentially damaging inflammatory processes PCOS causes in the body
Best Supplements for Polycystic Ovary Syndrome
The use of certain vitamins and minerals can be extremely useful in helping to correct Polycystic Ovary Syndrome, along with a good diet.
Chromium
Chromium helps to encourage the formation of glucose tolerance factor (GTF), which is required to make insulin more efficient. A deficiency of chromium can lead to insulin resistance. It also helps to control cravings and reduces hunger. This can help to reduce insulin resistance associated with PCOS
B vitamins
The B vitamins are very important in helping to control the symptoms of PCOS. Vitamin B2 helps to burn fat, sugar and protein into energy. B3 is a component of GTF which is released every time blood sugar rises, and vitamin B3 helps to keep the levels in balance. Vitamin B5 has been shown to help with weight loss and B6 is also important for maintaining hormone balance and, together with B2 and B3, is necessary for normal thyroid function.
Zinc
Zinc helps with PCOS as it plays a crucial role in the production of your reproductive hormones and also regulates your blood sugar.
Magnesium
Magnesium is an important mineral for dealing with PCOS because there is a strong link between magnesium levels and insulin resistance – the higher your magnesium levels the more sensitive you are likely to be to insulin.
Co-Enzyme Q10
Co-Q10 is a substance that your body produces in nearly every cell. It helps to balance your blood sugar and lowering both glucose and insulin.
Alpha lipoic acid
This powerful antioxidant helps to regulate your blood sugar levels because it releases energy by burning glucose and it also helps to make you more insulin sensitive. It also has an effect on weight loss because if the glucose is being used for energy, your body releases less insulin and you then store less fat.
Omega 3 fatty acids
Omega 3 fatty acids taken in supplement form have been found to reduce testosterone levels in women with Polycystic Ovary Syndrome.
Amino Acids
Certain amino acids can be very helpful for PCOS as they can improve your insulin sensitivity and also can have an effect on weight loss.
N-Acetyl cysteine
In women with PCOS this amino acid helps reduce insulin levels and makes your body more sensitive to insulin. Study using NAC in women who were clomiphene resistant and had ovarian drilling. After ovarian drilling, the women given NAC compared to a placebo showed a significantly higher increase in both ovulation and pregnancy rates and lower incidence of miscarriage.
Arginine
Arginine can be helpful in reversing insulin resistance. In one study, a combination of both arginine and N-acetyl cysteine was given to women with Polycystic Ovary Syndrome. The two amino acids help to improve blood sugar and insulin control and also increased the number of menstrual cycles and ovulation with one woman becoming pregnant in the second month.
Carnitine
Carnitine helps your body break down fat to release energy and can help improve insulin sensitivity.
Tyrosine
Tyrosine is helpful for women with PCOS who are overweight as it helps to suppress the appetite and burn off fat.
Glutamine
This amino acid is useful for helping with sugar cravings as it can be converted to sugar for energy and so takes away the need to eat something sweet. It also helps to build and maintain muscle which is important for fat burning.
Branched Chain Amino Acids (BCAAs)
BCAAs include the three amino acids leucine, isoleucine and valine. They are important in PCOS because they help to balance blood sugar and having good levels of these BCAAs can have a beneficial effect on your body weight
Inositol
A study used inositol (2,000mg) in combination with NAC (600mg), a significant increase in ovulation rates.
Having a good diet, regular exercise, controlling stress and taking key nutrients will help in getting your hormones back in balance and reducing the negative symptoms associated with PCOS.




