A difficult-to-diagnose pathology
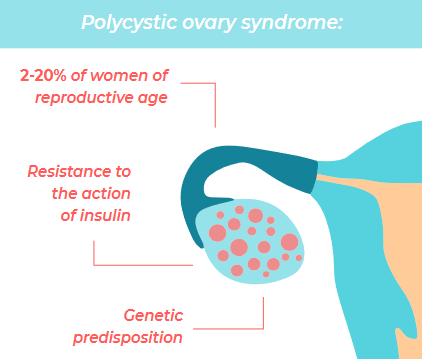
Polycystic ovary syndrome is the most frequent endocrine alteration in women of fertile age. This is a complex and sometimes difficult-to-diagnose condition that may affect a woman reproductively, metabolically and psychologically. Although the incidence may vary depending on race and diagnostic criteria, it is estimated that 2% to 20% of women of reproductive age may have it.
Despite the cause of its origin being unknown, it seems evident that there is a genetic predisposition to developing this syndrome that may presumably cause several members of the family to have it. Thus, it is not uncommon to find mothers and daughters or sisters affected within the same household. Furthermore, exposure to various environmental factors, including from foetal development during pregnancy, as well as lifestyle, seemingly contributes to the appearance of the syndrome in susceptible individuals.
Polycystic ovary syndrome is a metabolic disorder characterised by a resistance to the action of insulin (the hormone responsible for metabolising sugars within cells) and an increase in its concentration (hyperinsulinemia). This causes elevated blood sugar levels and makes women more likely to have an intolerance to sugar, diabetes mellitus or diabetes during pregnancy.
On the other hand, the association between polycystic ovary syndrome and obesity is frequent and may occur in up to 90% of patients. It is important to remember that obesity is an isolated risk factor for infertility and that it reduces the effectiveness of assisted reproduction treatments.
Although it is sometimes difficult to identify, several criteria must be met in order to establish the diagnosis of PCOS:
- Elevation of male hormone levels (hyperandrogenism). In 60% of women, this may produce an increase in body hair (hirsutis), alopecia or acne. Although in most cases the diagnosis is made by evaluating these signs, a specific test may sometimes be carried out to determine the level of male hormones. These signs, along with excess weight, obesity, or difficulties in becoming pregnant, means that the emotional impact on women suffering f rom polycystic ovary syndrome may be significant.
- Menstrual irregularities such as a lengthening of the cycle (oligomenorrhea) or absence of ovulation (anovulation), due to the metabolic alterations that have been described, may make it difficult to achieve pregnancy naturally. In addition, the risk of endometrial cancer may increase in patients who have not menstruated during many months, particularly in those who are obese.
- Ultrasound pattern of the polycystic ovary. This pattern is defined as a larger than usual ovaries with more than 12 antral follicles in each ovary. It is important not to confuse this pattern with an ovary with a good ovarian reserve, which is typical of young women.
Customised treatment
Treatment of PCOS must be individualised and sometimes involves several specialists, such as a gynaecologist, endocrinologist, dermatologist or nutritionist. As a general rule — and especially in patients who are obese or overweight — the recommendation is to have healthy lifestyle habits, a healthful diet and to exercise regularly. This will improve insulin sensitivity and decrease the production of male hormones, and promote ovulation, a regular menstrual cycle and an improvement in the hirsutism or acne. Several studies show that a loss of 5% to 10% of the initial weight is capable of improving metabolic parameters and restoring menstrual rhythm and ovulation in patients in which they were altered.
When establishing a therapeutic strategy, patients should be differentiated into two groups: those who do not wish to be pregnant, and those who do. Combined hormonal contraceptives may be used in patients who do not wish to become pregnant and have irregular rules, provided that there are no contraindications. They will help regulate the menstrual cycle, reducing the risk of endometrial cancer, and will reduce male hormone levels and their clinical manifestations. There are some specific preparations with antiandrogenic effects such as dienogest, cyproterone acetate and drospirenone.
Other treatment options for these patients are the use of progesterone in the second part of the menstrual cycle, contraceptives containing only progesterone, or the progesterone releasing IU.
On the other hand, drugs for inducing ovulation, such as clomiphene citrate, metformin, letrozole or gonadotropins will be used for women do wish to become pregnant. If the pregnancy is not achieved naturally after these drugs are administered, assisted reproduction techniques such as artificial insemination or in vitro fertilization may be used, depending on the characteristics of the patient or the couple. Special interest will be given to avoiding complications during treatment, such as ovarian hyperstimulation syndrome.