Obesity has a significantly negative effect on reproduction, affecting both women who seek gestation spontaneously and those who undergo assisted reproductive techniques.
In clinical practice, the simplest way to estimate the degree of obesity is based on the Body Mass Index (BMI), which is calculated by dividing a person’s weight in kilograms by the square of their height in meters. A person with a BMI between 18.5 and 25.9 Kg/m2 has an adequate weight, between 25.9 and 29.9 Kg/m2 is considered overweight, and when the BMI is equal to or greater than 30, they are considered obese.
Women with a BMI that is greater than 30 Kg/m2 have been observed to have three times more changes in their menstrual cycle than those with an adequate weight. This is because obesity produces a deregulation in the hypothalamic-pituitary-adrenal axis, altering the pulsatile secretion of GnRH and producing a preferential increase in LH with respect to FSH. This leads, on the one hand, to excessive secretion of testosterone and, on the other hand, to follicular arrest, ultimately leading to anovulation and amenorrhea. This clinical picture is usually typical in patients with polycystic ovary syndrome (PCOS), present in 75% of overweight women.
Obesity not only produces anovulatory problems but also has a direct harmful effect on oocytes, the subsequent development of embryos, and consequent implantation in the endometrium.
In assisted reproductive treatments, this translates into the need to apply a higher dose of gonadotropins, a higher percentage of cycles canceled as a result of poor response and, ultimately, a low success rate.
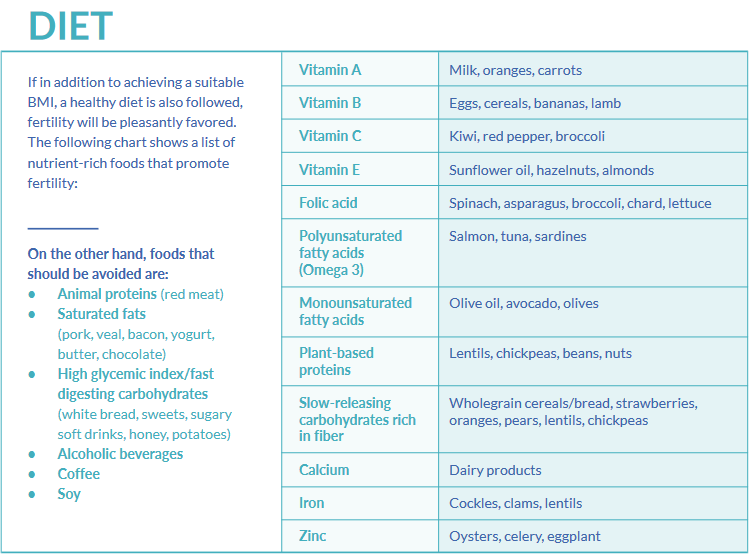
Despite some discrepancies between studies regarding the ratio of weight loss to rate of live births, it is apparent that a 5 to 10% weight loss causes a significant improvement at the endocrine level, thus achieving more regular menstrual cycles. It also means a lower dose of medication required, higher proportion of mature oocytes, better quality of embryos to be transferred, lower rate of miscarriage and preeclampsia, and the need for fewer cycles.
Therefore, weight loss should be the first therapeutic priority in these patients. And this should not only be the case in women, but should also apply to men, as existing studies today indicate that obesity also affects spermatogenesis, and with it, semen parameters (volume, concentration, vitality, mobility, and morphology).
The cause seems to be multifactorial in nature: excessive peripheral aromatization of testosterone to estradiol, insulin resistance, increased temperature in gonads, erectile dysfunction, reactive oxygen species (ROS), etc.