Does the human papillomavirus threaten my fertility?
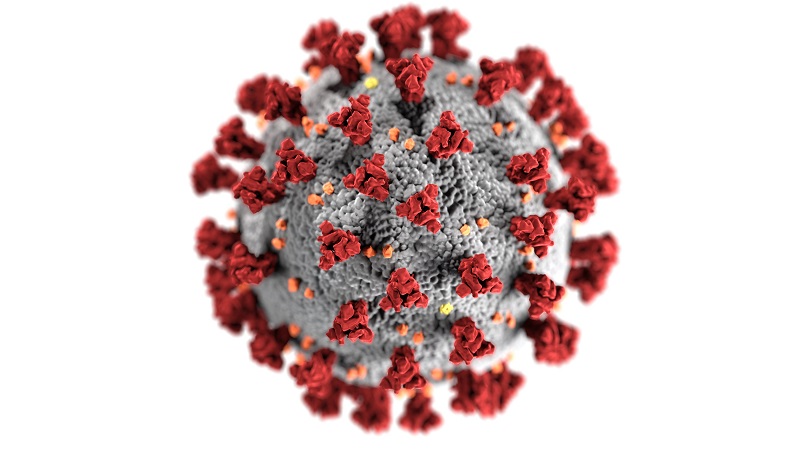
The human papillomavirus (HPV) is one of the world’s most widespread sexually transmitted infections. There are more than 200 types of human papillomavirus (VHP). Some 40 types can infect women’s and men’s genital areas: vulva, vagina, cervix, rectum, anus, penis and scrotum.
Genital HPV infections are common, but most people with HPV have no symptoms and feel perfectly well. Thus, they don’t even know that they’re infected and they disappear by themselves. However, some types of HPV may cause genital warts or certain types of cancer. In the last two decades, multiple studies have provided solid evidence that identifies the human papillomavirus (HPV) as the causative agent of practically all cases of cervical cancer and their precursor lesions.
There are more than 200 types of VHP
40 types de VHP can infect women’s and men’s genital areas; main cause
of cervical cancer
Is this condition a threat to pregnancy?
The papillomavirus is not a cause of sterility, provided the patient does their usual checks. A woman affected by the virus may become pregnant, and a woman who is pregnant may get the virus.
In cases where pre-cancerous lesions are found, one treatment alternative is cervical conisation. This is the removal of a cone-shaped section from outer part of the cervix. There is no reason for this procedure to cause problems of infertility, however, in exceptional circumstances, the cone may completely close the cervix and prevent the passage of sperm.
In pregnant women with a history of cervical conisation in which the cervix may be shortened, second-trimester miscarriages or premature births may increase. Nevertheless, this effect is controversial, since these types of complications are very common in the general population of pregnant women. There is no evidence that determines whether cervical cerclage (stitching) should be recommended based on obstetric clinical history or on ultrasound findings. According to each hospital’s protocol, cervical length can be monitored and treated based on the findings.
Is there a risk of transmission to the baby?
The risk of vertical transmission during the perinatal period or persistent infection in the newborn is very low. More often than not, the auto-immune system takes care of eliminating the virus naturally and without further complications. The transmission route may be intrauterine through the birth canal, or even post-natal. The greatest risk of transmission for the newborn is a history of genital warts during pregnancy, and not it passing through the birth canal. This is why a caesarean section is not considered indicated for finishing the pregnancy, unless the birth canal is obstructed by lesions or if vaginal delivery may cause excessive bleeding.
When this happens, it may cause warts in babies’ airways (trachea and bronchi) and lungs. This is called juvenile-onset recurrent respiratory papillomatosis. It is the most serious and is usually diagnosed between two and five years of age. There are no studies that determine the effect of treating warts in the transmission of the virus to the foetus. However, treatment is preferred over a wait-and-see approach. Treatment objective is to reduce the viral load, perinatal exposure and to prevent the growth and proliferation of lesions that may interfere in the birth. The main medical options are considered contraindicated. The recommended ones are CO2, cryotherapy, TCAA, excision and diathermic electrocoagulation.
When do you recommend getting vaccinated?
There are three vaccines for preventing HPV infection: Gardasil, Gardasil 9 and Cervarix. All three protect from infection by HPV types 16 and 18, two of the high-risk human papillomavirus that cause nearly 70% of cervical cancers. Even though these are inactivated vaccines, they must not be administered during pregnancy.
According to WHO, none of the vaccines is recommended during lactation. Although there are not enough studies on vaccination and the time to wait to try to get pregnant, the recommendation is one month after the last dose. If the vaccination schedule has begun but it not yet completed, there is one year to finish it. In addition, no teratogenicity or pregnancy complications have been shown in patients who were vaccinated without them knowing they were pregnant and so it is not a reason for pregnancy termination.